Esophageal spasms
Updated: 2024-11-09
Overview
Esophageal spasms are painful contractions in the muscular tube connecting the mouth and stomach, called the esophagus. Esophageal spasms can feel like sudden, bad chest pain that lasts from a few minutes to hours. Some people may mistake it for heart pain, also called angina.
Esophageal spasms usually happen only now and then, and they might not need treatment. But sometimes the spasms happen a lot and can prevent food and liquids from traveling through the esophagus. If esophageal spasms affect the ability to eat or drink, treatments are available.
Symptoms
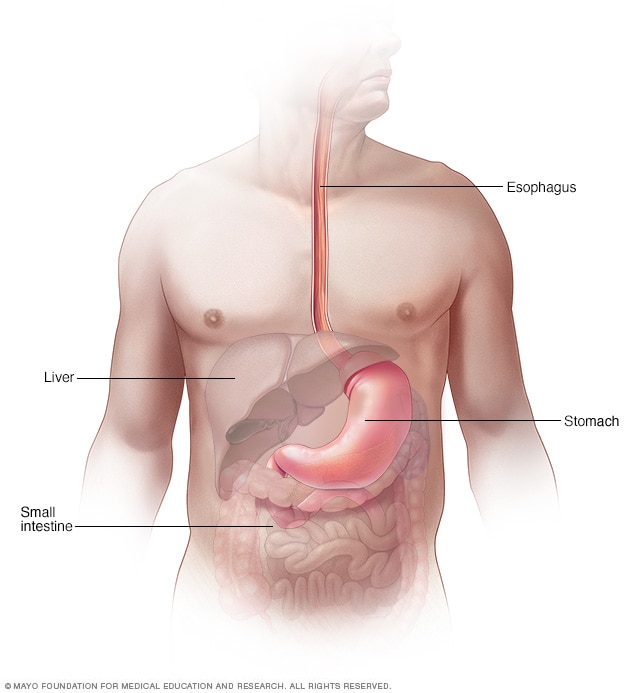
Esophagus
The esophagus is a muscular tube that connects the mouth and the stomach. Rings of muscle contract and relax to allow food and liquids to pass through the upper and lower portions.
Symptoms of esophageal spasms include:
- Squeezing pain in the chest. The pain is often intense and might be mistaken for heart pain or heartburn.
- Difficulty swallowing solids and liquids, sometimes related to swallowing specific substances. Red wine or extremely hot or cold liquids are more common culprits.
- The feeling that an object is stuck in the throat.
- The return of food and liquids back up the esophagus, also called regurgitation.
When to see a doctor
The squeezing chest pain that happens with esophageal spasms also can be caused by a heart attack. If you have squeezing chest pain, seek medical care right away.
Causes
It's not clear what causes esophageal spasms. However, they appear to be related to abnormal functioning of nerves that control the muscles used when swallowing.
A healthy esophagus moves food into the stomach through a series of coordinated muscle contractions. Esophageal spasms make it difficult for the muscles in the walls of the lower esophagus to coordinate. This makes it harder for the muscles to move food to the stomach.
There are two types of esophageal spasms — distal esophageal spasm and hypercontractile esophagus, also known as nutcracker esophagus.
Risk factors
Risk factors for esophageal spasms include:
- Sex. Women are more likely to have esophageal spasms than men.
- Age. Esophageal spasms tend to happen around age 60.
Diagnosis
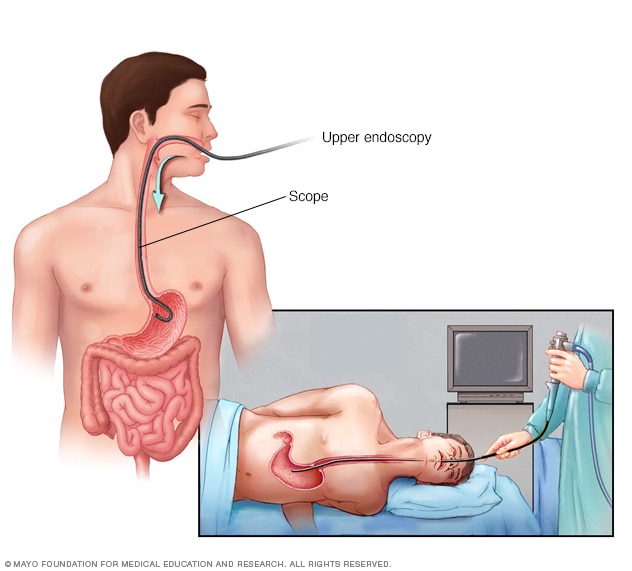
Endoscopy
During an upper endoscopy, a healthcare professional inserts a thin, flexible tube equipped with a light and camera down the throat and into the esophagus. The tiny camera provides a view of the esophagus, the stomach and the beginning of the small intestine, called the duodenum.
To diagnose esophageal spasms, a healthcare professional may recommend:
- Upper endoscopy. An upper endoscopy uses a tiny camera on the end of a flexible tube to visually examine the upper digestive system. Endoscopy also can be used to collect a sample of tissue to be tested for other esophageal diseases. This tissue sample is known as a biopsy.
- X-rays of the upper digestive system, also called an esophagram. X-rays are taken after drinking a chalky liquid that coats and fills the inside lining of the digestive tract. The coating allows a specialist to see a silhouette of the esophagus, stomach and upper intestine. Some people may experience loose stools for 1 to 2 days after this test.
- Esophageal manometry. This test measures the rhythmic muscle contractions in the esophagus when swallowing; the coordination and force exerted by the esophagus muscles; and how well the lower esophageal sphincter relaxes or opens during a swallow.
Treatment
Treatment depends on how often the esophageal spasms happen and how bad they are.
If the spasms only happen now and then, a healthcare professional might first recommend avoiding extremely hot or cold foods to see if that relieves symptoms.
If your spasms make it difficult to eat or drink, your provider might recommend:
- Managing any underlying conditions. Esophageal spasms are sometimes associated with conditions such as heartburn or gastroesophageal reflux disease (GERD). A healthcare professional might recommend a proton pump inhibitor to treat GERD. Sometimes an antidepressant, such as imipramine, may be prescribed. This medicine may help reduce the feeling of pain in the esophagus.
- Medicines to relax your swallowing muscles. Peppermint oil, onabotulinumtoxinA (Botox) injections into the esophagus or calcium channel blockers, such as diltiazem (Cardizem, Tiazac, others), can make spasms less severe.
- Surgery (myotomy). If medicine doesn't work, a healthcare professional might recommend a procedure that involves cutting the muscle at the lower end of the esophagus. This procedure, called a myotomy, can help weaken esophageal contractions. Long-term studies of this approach aren't available, so myotomy generally isn't recommended for esophageal spasms. However, it might be considered if other treatments don't work.
- Peroral endoscopic myotomy (POEM). The POEM procedure is minimally invasive. This newer technique involves placing an endoscope through the mouth and down the throat. This allows a surgeon to make a cut in the inside lining of the esophagus. Then, as in standard myotomy, the surgeon cuts the muscle at the lower end of the esophagus. Like standard myotomy, POEM is usually considered only if other treatments don't work.
Lifestyle and home remedies
To help you cope with occasional esophageal spasms, try to:
- Avoid your triggers. Make a list of foods and beverages that cause your esophageal spasms.
- Choose food that is warm or cool. Let foods and drinks that are very hot or very cold sit for a bit before eating or drinking them.
- Suck a peppermint lozenge. Peppermint oil is a smooth muscle relaxant and might help ease esophageal spasms. Place the peppermint lozenge under your tongue.
Preparing for an appointment
You may be referred to a healthcare professional who specializes in the digestive system, also called a gastroenterologist.
What you can do
- Be aware of any pre-appointment restrictions, such as fasting before your appointment.
- Write down your symptoms, including any that may seem unrelated to the reason you scheduled the appointment.
- Write down any triggers to your symptoms, such as specific foods.
- Make a list of all your medicines, vitamins and supplements.
- Write down your key medical information, including other conditions.
- Write down key personal information, including any recent changes or stressors in your life.
- Write down questions to ask during your appointment.
- Ask a relative or friend to accompany you, to help you remember what was discussed during the appointment.
Questions to ask your doctor
- What's the most likely cause of my symptoms?
- What tests do I need? Is there any special preparation for them?
- Is my condition likely temporary or long-lasting?
- What treatments are available?
- What types of foods are likely to make my symptoms worse?
- I have other health problems. How can I best manage these conditions together?
In addition to the questions that you've prepared, don't hesitate to ask other questions.
What to expect from your doctor
You're likely to be asked a few questions. Being ready to answer them may leave time to go over points you want to spend more time on. You may be asked:
- When did you begin experiencing symptoms? How severe are they?
- Have your symptoms been continuous or occasional?
- What, if anything, seems to improve or worsen your symptoms?
- Does exertion bring on your chest pain?
- Is your chest pain associated with arm or jaw pain, shortness of breath, or nausea?
- Are your symptoms related to eating? Are they triggered by any particular food or type of food?
- Do you experience symptoms of heartburn after eating, such as a burning sensation in your chest or an acid taste in your mouth?
- Do you ever wake up during the night with heartburn, chest pain or an acid taste in your mouth?
- Do you have difficulty swallowing food, or have you had to change your diet to avoid difficulty swallowing?