Burns
Updated: 2024-09-11
Overview

Second-degree burn
A second-degree burn often looks wet or moist. It affects the first and second layers of skin, which are called the epidermis and the dermis. Blisters may develop, and pain can be terrible.
Burns are tissue damage that results from too much sun, hot liquids, flames, chemicals, electricity, steam and other sources. Burns can be minor medical problems or life-threatening emergencies.
The treatment of burns depends on where they are on the body and how bad they are. Sunburns and small scalds can often be treated with first aid. Deep or widespread burns and chemical or electrical burns need medical care right away. Some people need treatment at specialized burn centers and monthslong follow-up care.
Symptoms
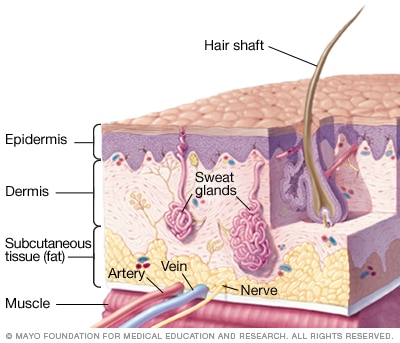
Skin anatomy
The skin has three layers that house sweat and oil glands, hair follicles, blood vessels, and the cells that give skin its color. These cells are called melanocytes.

Third-degree burn
Third-degree burns involve all of the layers of skin and sometimes the fat and muscle tissue under the skin. The skin may appear stiff, waxy white, leathery or gray. These types of burns often need skin grafts to close the wound.

Radiation burn
Radiation burns can be caused by X-rays or radiation therapy to treat cancer.
Burn symptoms vary depending on how deep the skin damage is. It can take a day or two for the symptoms of a severe burn to develop.
- First-degree burn, also called superficial burn. This minor burn affects only the outer layer of the skin, which is called the epidermis. It may cause pain and redness or other changes in skin color.
- Second-degree burn, also called partial-thickness burn. This type of burn affects both the epidermis and the second layer of skin, which is called the dermis. It may cause swelling and red, white or splotchy skin. Blisters may develop, and pain can be terrible. Deep second-degree burns can cause scarring.
- Third-degree burn, also called full-thickness burn. This burn involves all of the layers of skin and sometimes the fat and muscle tissue under the skin. Burned areas may be black, brown or white. The skin may look leathery. Third-degree burns can destroy nerves, so there may be little or no pain.
When to see a doctor
Call 911 or seek immediate care for:
- Burns that may be deep, involving all layers of the skin.
- Burns that cause the skin to be dry and leathery.
- Burns that look charred or have patches of white, brown or black.
- Burns that are larger than 3 inches (about 8 centimeters) wide.
- Burns that cover the hands, feet, face, neck, groin, buttocks or a major joint, or burns that encircle an arm or a leg.
- Difficulty breathing due to breathing in smoke or fumes.
- Headache or nausea due to exposure to fire and smoke.
- Burns that begin swelling very quickly.
- Major burns that were caused by chemicals, gunpowder or an explosion.
- Electrical burns, including those caused by lightning.
- A sunburn with a fever greater than 103 degrees Fahrenheit (39 degrees Celsius) and vomiting.
- An infection over a sunburned area.
- A sunburn with confusion or passing out.
- A sunburn with dehydration.
Take first-aid measures while waiting for emergency assistance.
A minor burn might need emergency care if it affects the eyes, mouth, hands or genitals. Babies and older adults might need emergency care for minor burns as well.
Call your healthcare professional if you experience:
- Signs of infection, such as oozing and streaks from the wound, and fever.
- A burn or blister that's wider than 2 inches (about 5 centimeters) or doesn't heal in two weeks.
- New symptoms that can't be explained.
- A burn and also have a history diabetes.
Also call your health professional if you think you might need a tetanus booster. You may need a booster shot if you haven't had a tetanus shot in the past five years. Try to get this within three days of the injury.
Causes
Burns are caused by:
- Fire.
- Hot liquid or steam.
- Hot metal, glass or other objects.
- Electrical currents.
- Nonsolar radiation, such as that from X-rays.
- Sunlight or other sources of ultraviolet radiation, such as tanning beds.
- Chemicals such as strong acids, lye, paint thinner or gasoline.
- Abuse.
Risk factors
Risk factors for burns include:
- Workplace factors. People who work outdoors and people who work with flames, chemicals and other substances that cause burns are at increased risk of burns. Most burns occur in adults.
- Dementia. Older adults with dementia are more likely to have burns from heat sources, such as too-hot tap water, hot drinks, food fats and cooking oils.
- Being young. Very young children are unable to get away from heat sources or flames. Their burns often come from kitchen, car seat and bath hazards.
- Alcohol. Risk of burns is increased among people who drink alcohol or use other substances that affect judgment.
Complications
Complications of deep or widespread burns can include:
- Infection. Examples include bacterial infection, tetanus, and pneumonia.
- Fluid loss. This includes low blood volume, which is also known as hypovolemia.
- Dangerously low body temperature. This is known as hypothermia.
- Breathing problems. These can occur after taking in hot air or smoke.
- Irregular heartbeats. Also called arrythmias, irregular heartbeats can occur after electrical burns.
- Scars and changes in skin color. Scars or ridged areas can be caused by an overgrowth of scar tissue. These types of scars are called hypertrophic scars or keloids. Black people have an increased risk of this type of scarring and may benefit from seeing a burn specialist or surgeon. Other people may develop skin color changes after burns if healed skin is lighter or darker than skin that wasn't burned.
- Pain. Burn scars can be painful. Some people may experience itching or discomfort related to damaged nerves, causing numbness or tingling.
- Bone and joint problems. Scar tissue can shorten and tighten skin, muscles or tendons. This condition is also known as a contracture.
- Depression and anxiety disorders.
- Skin cancer. Skin cancer can sometimes happen in scars from previous burns. Contact your healthcare professional if you notice a sore that isn't healing within a burn scar.
Prevention
Burns are very common, and most of them are preventable. Kitchen-related injuries from hot drinks, soups and microwaved foods are especially common among children. You can take steps to reduce the risk of household burns.
Kitchen, car seat and bath hazards
- Never leave items cooking on the stove unattended.
- Turn pot handles toward the rear of the stove, or cook on the back burners.
- Don't carry or hold a child while cooking at the stove.
- Keep hot liquids out of the reach of children and pets.
- Check the temperature of food before serving it to a child. Don't heat a baby's bottle in the microwave.
- Never cook while wearing loose-fitting clothes. They could catch fire over the stove.
- If small children are present, block their access to heat sources. Examples include stoves, outdoor grills and fireplaces.
- Before placing a child in a car seat, check for hot straps or buckles.
- Set your water heater's thermostat to below 120 degrees Fahrenheit (48.9 degrees Celsius) to prevent scalding. Older adults and young children are at increased risk of burns from tap water. Always test bathwater before using it.
Electrical devices
- Unplug irons, space heaters and similar devices when not in use. Store them out of reach of small children.
- Keep electrical appliances away from water.
- Cover unused electrical outlets with safety caps.
- Keep electrical cords and wires out of the way so that children can't chew on them.
Fire prevention
- If you smoke, quit. If you don't quit, never smoke in bed.
- Blow out candles before leaving the room or sleeping.
- Be sure you have working smoke detectors on each floor of your home. Check them and change their batteries at least once a year.
- Keep a fire extinguisher handy and learn how to use it.
Chemical hazards
- When using chemicals, always wear protective eyewear and clothing.
- Keep chemicals, lighters and matches out of the reach of children. Use safety latches. And don't use lighters that look like toys.
Diagnosis
If you go to a healthcare professional for burn treatment, the health professional figures out how bad your burn is by examining your skin. You may be transferred to a burn center if your burn covers more than 10% of your total body surface area, is very deep, is on the face, feet or groin, or meets other criteria established by the American Burn Association.
Your healthcare professional also checks for other injuries and might order lab tests, X-rays or other diagnostic tests.
Treatment
Most minor burns can be treated at home. They usually heal within a couple of weeks.
For major burns, after first aid and after a healthcare professional looks at your burns, treatment may involve one or more of the following: medicines, wound dressings, therapy and surgery. The goals of treatment are to control pain, remove dead tissue, prevent infection, lower scarring risk and restore function.
People with major burns may require treatment at specialized burn centers. They may need skin grafts to cover large wounds. And they may need emotional support and months of follow-up care, such as physical therapy.
First aid for major burns
For major burns, apply first aid until emergency help arrives:
- Protect the burned person from further harm. If you can do so safely, make sure the person you're helping is not in contact with the source of the burn.
- Make certain that the burned person is breathing. If needed, begin rescue breathing if you know how.
- Remove jewelry, belts and other tight items, especially from the burned area and the neck. Burned areas swell quickly.
- Cover the burn. Loosely cover the area with gauze or a clean cloth.
- Raise the burned area. Lift the wound above heart level if possible.
- Watch for symptoms of shock. Symptoms include cool, clammy skin, weak pulse and shallow breathing.
Medical treatment
Medicines and products that may help with healing major burns include:
- Water-based treatments. Your care team may use techniques such as whirlpool baths to help remove dead tissue.
- Fluids to prevent dehydration. You may need intravenous fluids to prevent dehydration and organ failure. These also are called IV fluids.
- Pain and anxiety medicines. Healing burns can be incredibly painful. You may need morphine and anti-anxiety medicine. These also might be needed when your bandages are changed.
- Burn creams and ointments. If you aren't transferred to a burn center, your care team may use a variety of topical products for wound healing. Examples are bacitracin and silver sulfadiazine (Silvadene). These help prevent infection and prepare the wound to close.
- Dressings. Your care team also may use various specialty wound dressings to prepare the wound to heal. If you're being transferred to a burn center, your wound will likely be covered in dry gauze only.
- Drugs that fight infection. If you develop an infection, you may need IV antibiotics.
- Tetanus shot. Your healthcare team might tell you to get a tetanus shot after a burn injury.
Physical and occupational therapy
If the burned area is large or covers any joints, you may need to do physical therapy exercises. These can help stretch the skin so that the joints remain flexible. Other types of exercises can improve muscle strength and coordination. And occupational therapy may help if you have difficulty doing your daily activities.
Surgery and other treatments
You may need one or more of the following:
- Breathing assistance. If you've been burned on the face or neck, your throat may swell shut. If that appears likely, a doctor may insert a tube down your windpipe, also called the trachea, to keep oxygen supplied to your lungs.
- Feeding tube. If you have burns over a large area or are undernourished, you may need nutritional support. A healthcare professional may thread a feeding tube through your nose to your stomach.
- Easing blood flow around the wound. If a burn scab, also called eschar, goes completely around a limb, it can tighten and cut off blood flow. An eschar that goes completely around the chest can make it hard to breathe. A healthcare professional may cut the eschar to ease this pressure.
- Skin grafts. A skin graft is a surgery that uses sections of your own healthy skin to replace the scar tissue caused by deep burns. Donor skin from deceased donors or pigs can be used for a short time.
Self care
For minor burns, follow these first-aid guidelines:
- Prevent further harm. Move away from whatever caused the burn. For sunburn, get out of the sun.
- Cool the burn. Hold the area under cool — not cold — running water for 10 to 20 minutes. If this isn't possible or if the burn is on the face, apply a cool, wet cloth until the pain eases. For a mouth burn from hot food or drink, put a piece of ice in the mouth for a few minutes.
- Remove rings or other tight items. Try to do this quickly and gently, before the burned area swells.
- Apply lotion. After the burn is cooled, apply a lotion, such as one with aloe vera or cocoa butter. This helps prevent drying and provides relief.
- Bandage the burn. Cover the burn with a clean bandage. Wrap it loosely to avoid putting pressure on burned skin. Bandaging keeps air off the area, reduces pain and protects blistered skin.
- If needed, take a pain reliever. Pain medicine you can buy without a prescription can help lessen pain. Examples include ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others).
Whether your burn was minor or serious, use sunscreen and moisturizer regularly once the wound is healed.
What not to do
- Don't use cold water to cool the burn.
- Don't break blisters. B listers help protect against infection. If a blister does break, gently clean the area with water and, if you wish, liquid soap. Apply an antibiotic ointment. If a rash appears, stop using the ointment.
- Don't use a fluffy cotton bandage.
- Don't apply ointments, grease, butter or pain-killing lotions.
- Don't try to remove clothing stuck in the burn.
Coping and support
Coping with a serious burn injury can be a challenge, especially if it covers large areas of the body or is in places readily seen by other people, such as the face or hands. Potential scarring, less mobility and possible surgeries add to the burden.
Consider joining a support group of other people who have had serious burns and know what you're going through. You may find comfort in sharing your experience and troubles and meeting people who face similar challenges. Ask your healthcare professional for information on support groups in your area or online.
Preparing for an appointment
Seek emergency medical care for burns that are deep or involve your hands, feet, face, groin, buttocks, a major joint or a large area of your body. Your healthcare team may recommend an exam by a skin specialist, burn specialist, surgeon or other specialist.
For other burns, you may need an appointment with your family healthcare professional. The information below can help you prepare.
List questions you want to ask your healthcare professional, such as:
- Do I need treatment for the burn?
- What are my treatment options and the pros and cons of each?
- What are the alternatives to the primary approach that you're suggesting?
- Can I wait to see if the burn heals on its own?
- Do I need prescription medicine, or can I use nonprescription medicines to treat the burn?
- What results can I expect?
- What skin care routines do you recommend while the burn heals?
- What kind of follow-up, if any, will I need?
- What changes in my skin might I expect to see as it heals?
What to expect from your doctor
Your healthcare professional is likely to ask you a number of questions, such as:
- How did the burn occur?
- Do you have other symptoms?
- Do you have other health conditions, such as diabetes?
- What at-home burn treatments have you used, if any?
- Have you noticed any changes in the appearance of the burn?