Peptic ulcer
Updated: 2024-08-16
Overview
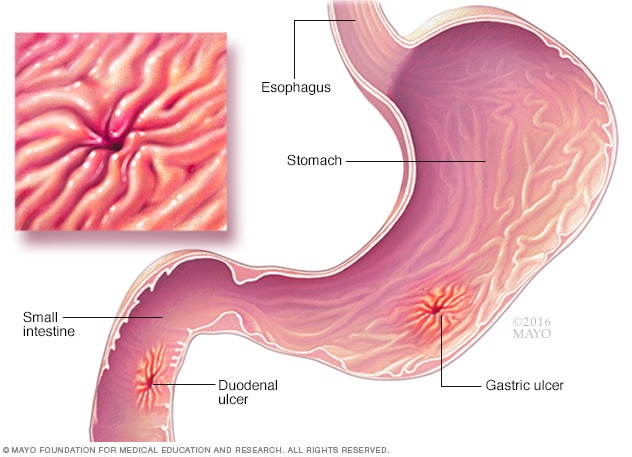
Ulcers
Peptic ulcers are open sores on the inner lining of the stomach and the upper part of the small intestine. A peptic ulcer in the stomach is called a gastric ulcer. A duodenal ulcer is a peptic ulcer that appears in the first part of the small intestine, called the duodenum.
Peptic ulcers are open sores on the inner lining of the stomach and the upper part of the small intestine. The most common symptom of a peptic ulcer is stomach pain.
Peptic ulcers include:
- Gastric ulcers, which appear on the inside of the stomach.
- Duodenal ulcers, which appear on the inside of the upper part of the small intestine, called the duodenum.
The most common causes of peptic ulcers are infection with the germ Helicobacter pylori (H. pylori) and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs). These include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
Stress and spicy foods do not cause peptic ulcers. But they can make symptoms worse.
Symptoms
Many people with peptic ulcers don't have symptoms. If there are symptoms, they may include:
- Dull or burning stomach pain. For some people, pain may be worse between meals and at night. For others, it may be worse after eating.
- Feeling of fullness or bloating.
- Belching.
- Heartburn.
- Nausea.
Peptic ulcers can cause bleeding from the ulcer. Then symptoms might include:
- Vomiting blood, which may appear red or black.
- Having dark blood in stools, or stools that are black or tarry.
- Feeling dizzy or fainting.
When to see a doctor
See your healthcare professional if you're vomiting blood, having dark blood in stools or are feeling dizzy. Also see your healthcare professional if nonprescription antacids and acid blockers relieve your pain but the pain returns.
Causes
Peptic ulcers happen when acid in the organs that food travels through, called the digestive tract, eats away at the inner surface of the stomach or small intestine. The acid can create a painful open sore that may bleed.
Your digestive tract is coated with a mucous layer that most often protects against acid. But if the amount of acid increases or the amount of mucus decreases, you could develop an ulcer.
Common causes include:
-
Helicobacter pylori. This germ lives in the mucous layer that covers and protects tissues that line the stomach and small intestine. The H. pylori germ often causes no problems. But it can cause swelling and irritation, called inflammation, of the stomach's inner layer. When this happens, it can cause an ulcer.
It's not clear how H. pylori infection spreads. It may go from person to person by close contact, such as kissing. People also can contract H. pylori through food and water.
- Regular use of certain pain relievers. Taking aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) over time can irritate or inflame the lining of the stomach and small intestine. These medicines include ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, Anaprox DS, others), ketoprofen and others. They do not include acetaminophen (Tylenol, others).
Risk factors
If you take NSAIDs, the following factors may increase your risk of peptic ulcers:
- Old age. This includes people older than 60.
- Prior peptic ulcer. People who have had a peptic ulcer before have a higher risk of having another one.
NSAIDs use. Taking high doses of NSAIDs or two or more NSAIDs increases the risk. So does taking NSAIDS with certain other medicines.
These include other pain relievers, steroids, blood thinners, certain antidepressants called selective serotonin reuptake inhibitors (SSRIs) and medicines to treat the bone-thinning disease osteoporosis. These include alendronate (Fosamax, Binosto) and risedronate (Actonel, Atelvia).
Factors that don't cause peptic ulcers but can make them worse include:
- Smoking. This may increase the risk of peptic ulcers in people who are infected with H. pylori.
- Drinking alcohol. Alcohol can irritate and erode the mucous lining of the stomach. And it increases stomach acid.
- Having untreated stress.
- Eating spicy foods.
Complications
Untreated peptic ulcers can cause:
- Bleeding in the stomach or duodenum. Bleeding can be a slow blood loss that leads to too few red blood cells, called anemia. Or you can lose enough blood so that you need to be in a hospital or get blood from a donor. Severe blood loss may cause black or bloody vomit or black or bloody stools.
- A hole, called a perforation, in the stomach wall. Peptic ulcers can eat a hole through the wall of your stomach or small intestine. This puts you at risk of infection of your abdomen, called peritonitis.
- Blockage. Peptic ulcers can keep food from going through the digestive tract. The blockage can make you feel full easily and cause you to vomit and lose weight.
- Stomach cancer. Studies have shown that people infected with H. pylori have an increased risk of stomach cancer.
Prevention
To help prevent peptic ulcers:
-
Take care with pain relievers. If you often use NSAIDs, which can increase your risk of peptic ulcer, take steps to reduce your risk of stomach problems. For instance, take pain relievers with meals.
Work with your healthcare professional to find the lowest dose that gives you pain relief. Don't drink alcohol with pain relievers. Together, they can increase your risk of stomach upset.
If you need an NSAID, you also may need to take other medicines to help protect your stomach. These include antacids, proton pump inhibitors, acid blockers or cytoprotective agents.
A class of NSAIDs called COX-2 inhibitors may be less likely to cause peptic ulcers. But these medicines may increase the risk of heart attack.
- If you smoke, find a way to quit. Quitting smoking can lower your risk of peptic ulcer. Talk with your healthcare professional for help with quitting.
Diagnosis
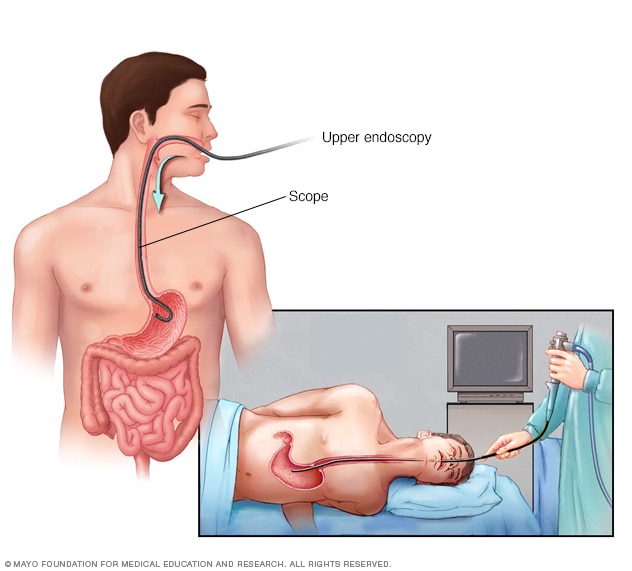
Upper endoscopy
During an upper endoscopy, a healthcare professional inserts a thin, flexible tube equipped with a light and camera down the throat and into the esophagus. The tiny camera provides a view of the esophagus, stomach and the beginning of the small intestine, called the duodenum.
To detect an ulcer, your healthcare professional may first take a medical history and do a physical exam. You also may need tests, such as:
-
Laboratory tests for H. pylori. A blood, stool or breath test can show whether H. pylori is in your body.
For the breath test, you drink or eat something that contains radioactive carbon. H. pylori breaks down the substance in your stomach. Later, you blow into a bag, which is then sealed. If you have H. pylori, your breath sample has the radioactive carbon in the form of carbon dioxide.
If you take an antacid or an antibiotic, tell your healthcare professional. You may need to stop the medicine for a time. Both can affect test results.
-
Endoscopy. During this procedure, your healthcare professional uses a long, flexible tube with a tiny camera, called an endoscope, to look at the upper part of your digestive system. Endoscopy involves passing the endoscope, down your throat and into your esophagus, stomach and small intestine to look for ulcers.
If there's an ulcer, your health professional may remove a small tissue sample for study in a lab. This is called a biopsy. A biopsy also can show whether H. pylori is in your stomach lining.
You're more likely to have endoscopy if you are older, have signs of bleeding, or have had recent weight loss or trouble eating and swallowing. If the endoscopy shows an ulcer in your stomach, you're likely to have a follow-up endoscopy after treatment. This can show if the ulcer has healed.
- Upper gastrointestinal series. Sometimes called a barium swallow, this series of X-rays of the upper digestive system makes pictures of your esophagus, stomach and small intestine. During the series of X-rays, you swallow a white liquid that has barium. The liquid coats your digestive tract and makes an ulcer easier to see.
Treatment
Treatment for peptic ulcers involves killing the H. pylori germ, if needed. Treatment also might involve stopping NSAIDs or lowering the amount, if possible, and taking medicine to help the ulcer heal.
Medicines can include:
- Antibiotics to kill H. pylori. If you have H. pylori in your digestive tract, your healthcare professional may suggest a mix of antibiotics. These may include amoxicillin (Amoxil, Larotid), clarithromycin (Biaxin XL), metronidazole (Flagyl, Likmez), tinidazole (Tindamax), tetracycline and levofloxacin.
-
Medicines that block acid. Proton pump inhibitors (PPIs) reduce stomach acid. PPIs include omeprazole (Prilosec), lansoprazole (Prevacid), rabeprazole (Aciphex), esomeprazole (Nexium) and pantoprazole (Protonix).
Most people take PPIs in pill form. In the hospital, treatment for a bleeding ulcer may involve a PPI given through a vein in the arm. This is known as intravenous delivery.
Long-term or high-dose use of proton pump inhibitors may increase your risk of hip, wrist and spine fracture. Ask your healthcare professional whether a calcium supplement may reduce this risk.
- Medicines to reduce stomach acid. Acid blockers, also called histamine (H-2) blockers, help relieve ulcer pain and help with healing. Acid blockers include famotidine (Pepcid AC), cimetidine (Tagamet HB) and nizatidine (Axid AR).
- Antacids that counter the effects of stomach acid. These can relieve pain quickly. But they aren't used to heal ulcers. Side effects can include constipation or diarrhea, depending on the main ingredients in the antacids.
- Medicines that protect the lining of the stomach and small intestine. These are called cytoprotective agents. They include the prescription medicines sucralfate (Carafate) and misoprostol (Cytotec).
Follow-up after treatment
Treatment for peptic ulcers often leads to ulcer healing. But if your symptoms are severe or if you have them even with treatment, your healthcare professional may suggest endoscopy. This procedure can rule out other possible causes for your symptoms.
If your healthcare professional finds an ulcer during endoscopy, you may need another endoscopy after your treatment to make sure your ulcer has healed.
Ulcers that don't heal
Peptic ulcers that don't heal with treatment are called refractory ulcers. Reasons for an ulcer not healing include:
- Not taking medicines as prescribed.
- Having a type of H. pylori that resists antibiotics.
- Often using pain relievers, such as NSAIDs, that increase the risk of ulcers.
Less often, refractory ulcers may be a result of:
- A lot of stomach acid, such as happens in Zollinger-Ellison syndrome.
- An infection other than H. pylori.
- Stomach cancer.
- Other conditions that may cause ulcerlike sores in the stomach and small intestine, such as Crohn disease.
Treatment for refractory ulcers most often involves getting rid of factors that keep the ulcer from healing and trying other antibiotics. If you smoke, your healthcare professional may suggest you quit. Smoking can slow ulcer healing.
A serious complication from an ulcer, such as bleeding or a hole in the stomach, may need treatment with endoscopy or surgery. But because there are many medicines that work well, people with peptic ulcers need surgery far less often than in the past.
Lifestyle and home remedies
You may find relief from the pain of a stomach ulcer if you:
- Switch pain relievers. If you use pain relievers regularly, ask your healthcare professional whether acetaminophen (Tylenol, others) might work for you.
- Control stress. Stress may make the symptoms of a peptic ulcer worse. Think about what causes your stress and what you can do to ease it. There are many ways to cope with stress. These include exercise, spending time with friends, deep breathing, writing in a journal or meditating.
- Don't smoke. Smoking may harm the lining of the stomach, raising the chance of getting an ulcer. Smoking also increases stomach acid.
- Limit or avoid alcohol. Too much alcohol can irritate and eat away the mucous lining in your stomach and intestines. This can cause the lining to inflame and bleed.
Alternative medicine
Products containing bismuth may help with symptoms of a peptic ulcer. There also is some evidence that zinc can help heal ulcers.
Talk to your healthcare professional before using any alternative medicine for peptic ulcers.
Preparing for an appointment
Make an appointment with your main healthcare professional if you have symptoms that worry you. Your health professional may send you to a specialist in the digestive system, called a gastroenterologist.
Here's information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet or stop certain medicines.
Make a list of:
- Your symptoms, when they began and whether they're worse when your stomach is empty.
- Key personal information, including any other medical concerns, major stresses or recent life changes. Include family history of peptic ulcers, H. pylori infection and cancer in the digestive tract.
- All medicines, vitamins or supplements you take, including doses. Be sure to include any pain relievers you use, how much you take and how often you take them.
- Write down questions to ask your healthcare professional.
For peptic ulcers, some questions to ask include:
- What's the most likely cause of my symptoms?
- What tests do I need? How do I prepare for them?
- Is my condition likely to go away or to last?
- What treatment do you suggest?
- Do I need to restrict my diet?
- I have other medical conditions. How can I manage these along with ulcers?
Be sure you ask all the questions you have.
What to expect from your doctor
Your healthcare professional might ask:
- Do you always have symptoms, or do they come and go?
- How bad are your symptoms?
- Are your symptoms worse when you're hungry?
- Does anything seem to improve your symptoms?
- Does anything make your symptoms worse?
- Do you have nausea? Have you been vomiting?
- Have you ever vomited blood or black material?
- Have you noticed blood in your stool or black stools?
What you can do in the meantime
While you wait for your appointment, don't use tobacco or alcohol or eat spicy foods to help ease your discomfort.